Main present positions
- ✔ Vice Medical Director, Division of Palliative Medicine Chief Director, Higashi Sapporo Hospital
- ✔ Clinical Professor, Department of Anesthesiology, Sapporo Medical University since 2008.
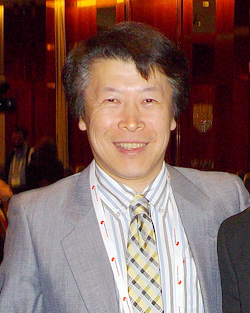
Bio-sketch
Born the 10th of April 1962, Kazuhiko Koike graduated from Sapporo Medical College at 1988 and chose Oncology section (Clinical Oncology, Gastroenterology, and Hematology) of Internal medicine (Section 4) of Sapporo Medical College. He hold Ph.D. from Sapporo Medical University (obtained in Jan 2003). His research has focused on the molecular mechanisms of cancer metastasis. His clinical and research experience include chemotherapy for cancer patients, supportive, and palliative care in cancer.
Currently he is vice medical director, and division of palliative care medicine chief director at Higashi Sapporo Hospital, where he has been providing comprehensive medical oncology and palliative care. In 2011 he was appointed as the chair of the organizing Committee in the 16th Congress of the Japanese Society for Palliative Medicine (JSPM). He is a Provisional Board Certified Senior Member of the JSPM and Chief executive officer of association for Palliative Medicine of Hokkaido. He has been elected in 2014 as Delegate to the JSPM. He is the Board Certified Gastroenterologist of The Japanese Society of Gastroenterology, and the Board of the Japanese Society of Internal Medicine. He is appointed as a palliative medicine section member of planning committee for the 13th Annual Meeting of Japanese Society of Medical Oncology in 2015.
Recent Publications (Peer-Reviewed Original Research Articles)
- 1. Koike K, Terui T, Takahashi Y, Hirayama Y, Mizukami N, Yamakage M, Kato J, Ishitani K: Effectiveness of multidisciplinary team conference on decision-making surrounding the application of continuous deep sedation for terminally ill cancer patients. Palliat Support Care. 2013 Nov 4: 1-8. [Epub ahead of print]
- 2. Terui T, Koike K, Hirayama Y, Kusakabe T, Ono K, Mihara H, Kobayashi K, Takahashi Y, Nakajima N, Kato J, Ishitani K: Recent Advances in Palliative Cancer Care at a Regional Hospital in Japan. Am J Hosp Palliat Care 2013 Sep 10. [Epub ahead of print]
- 3. Hirayama Y, Terui T, Kusakabe T, Koike K, Ono K, Kato J, Ishitani K: A Survey of Patients Who Were Referred to Our Palliative Care Division From Other Hospitals and Appeared to Have Obvious Indications for Cancer Chemotherapies. Am J Hosp Palliat Care 2013 Oct. 16. [Epub ahead of print]
- 4. Mizukami N, Yamauchi M, Koike K, Watanabe A, Ichihara K, Masumori N, Yamakage M : Olanzapine for the Prevention of Chemotherapy-Induced Nausea and Vomiting in Patients Receiving Highly or Moderately Emetogenic Chemotherapy: A Randomized, Double-Blind, Placebo-Controlled Study. J Pain Symptom Manage 2013 May. [Epub ahead of print]
[Additional comment]
Palliative Sedation and Qualities of Palliative Care
Abstract
Palliative sedation (PS) is a way to reduced conscious experience of refractory symptoms of severe suffering in terminally ill cancer patients. For patients suffering from severe pain, dyspnea, or other symptoms that prove refractory to treatment, there is consensus that palliative sedation is an appropriate intervention of last resort. It is assumed that all efforts to provide comfort have been exhausted and only sedating the patient to the point of unconsciousness until death, can be of benefit. PS will come to be seen as an alternative to providing high quality palliative care. High quality palliative care is an essential pre-condition for any consideration of palliative sedation and in fact, all palliative therapies must be exhausted, including treatment for pain, breathlessness, delirium and anxiety prior to using palliative sedation.
However, there are many medical and ethical misconceptions concerning the indications, procedure, and course of palliative sedation. How is “refractory” defined? Symptoms are defined as refractory if all other possible treatments have failed, or it is estimated by team consensus, based on repeated and careful assessments by skilled experts.
PS should only be administered safely and appropriately when multidisciplinary team is involved in the decision-making process. In our hospital, prior to administration of PS, MDTC was performed all the patients who will be considered to received PS by the attending physician. Of all 1581 deceased patients, 22(1.39%) had received PS. Six patients (0.38%) did not meet the appropriate criteria for PS according to the MDTC and, therefore, did not receive. Our results indicate that prevalence of PS will be decreased when carried out in an appropriate indication (1).
A multidisciplinary team approach to assessment and treatment is mandatory. Successful palliative care requires attention to all aspects of a patient’s suffering. This requires input or assistance from a range of medical, nursing and allied health personnel—a multidisciplinary approach. Continuity of teamwork, good coordination, exchange of information, and communication between the various care providers are essential on the decision-making process for palliative sedation. Lack of any of these may lead to inadequate assessment, information discrepancies, and distress.
(1) Koike K, et al: Effectiveness of multidisciplinary team conference on decision-making surrounding the application of continuous deep sedation for terminally ill cancer patients. Palliat & Support Care. 2013 Nov 4: 1-8. [Epub ahead of print]
